A cardiac arrest survival formula
With perfect understanding of all the factors and their influence on survival, plus whatever factors are yet to be identified, one could construct a formula giving the exact probability of survival from cardiac arrest. Such a global formula would be of academic interest and could help to understand variance (the difference between predicted survival and what actually occurs) in the formula and thereby allow exploration of additional predictive factors. A global formula would also allow family members to understand why a loved one did not survive cardiac arrest. In terms of system performance, however, a more meaningful formula would be one that focuses on factors that can be readily changed or influenced by community decisions. Of all 50 factors, the patient and event factors are set in stone. They are largely determined by fate or circumstances and not easily altered by EMS programmatic structure or therapeutic decisions at the scene. It is not possible to alter ones gender and not much can be done at the time of arrest to change body mass index or co-morbid factors. Similarly whether the collapse is witnessed and the rhythm at the time of arrest are hardly factors that one has control over. Such is not the case with system and therapy factors. These are directly determined by the type of EMS system and the multitude of decisions made by administrators, medical directors, and personnel at the scene.
A system and therapy focused survival formula would allow a community to instantly visualize where it succeeds or falls short. This formula would contain all the known system and therapy factors that determine survival from witnessed VF. Actually such a list is rather short. There is the time to CPR, the time to defibrillation, the interaction of CPR and defibrillation, timely and skilled paramedic care, and the institution of hypothermia for patients who achieve a pulse and blood pressure but do not wake up. These five factors are determinants of survival. All other factors are contributory factors in that they indirectly lead to improved survival. Iíve arbitrarily set the highest likely survival rate for any community as 50%. This is not an absolute ceiling and as better therapy and methods of delivery are derived this rate may be set higher. But for now the best systems in the United States (Seattle, King County, and Rochester, MN) report 46% survival rates for witnessed VF.
The following formula is admittedly a model and generalization and is based on a moderate amount of science combined with a fair amount of conjecture and estimate. Even if the formula is inexact, its thrust should be clear. With these qualifications in mind, here is how the formula might look:
Likelihood of survival from witnessed VF (maximum of 50%) is the average time to CPR (scored as follows: 15% for 4 minutes, 10% for 5 minutes, 5% for 6 minutes) plus the average time to first shock (scored as follows: 20% for 6 minutes, 15% for 7 minutes, 10% for 8 minutes, 5% for 9 minutes) plus 5% for carefully monitored interaction of CPR and defibrillation minimizing the time without CPR, plus 5% for timely delivery of skilled paramedic care, plus 5% if hypothermia is started within 2 hours of collapse in greater than 50% of cases. The times to CPR and defibrillation are the times from collapse to each of these interventions. They are not response times or time to scene. When bystanders begin CPR this time is arbitrarily designated as 50% of the interval from 911 pick-up to first-in unit at the address. According to this formula King County would receive 20% for CPR, 15% for defibrillation, 5% for interaction of CPR and defibrillation, 5% for timely and skilled paramedic care, and 0% for hypothermia -- total equals 45% -- spot on with the current survival rate. The interaction of CPR and defibrillation refers to the timing and sequence of defibrillation as well as the quality of CPR and defibrillation. New recording monitors can now accurately monitor the quality of CPR. Hypothermia is only beginning to become standard of care in King County as of 2007.
It deserves repeating that the formula is more a model than a precise survival calculator. It includes several arbitrarily assigned numbers (I like to think of them as educated estimates). The 5% each for CPR/defibrillation interaction, timely and skilled paramedic care, and hypothermia cannot be precisely quantified at this time. I must emphasize that this formula has not been validated and is based only on observational data. It may not apply to all communities. Nevertheless it is a good approximation of what is determinant of survival and what it takes to achieve a high score.
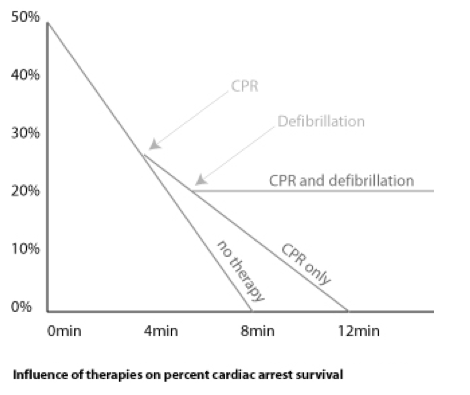
The cardiac arrest survival formula can be graphically represented. To understand the graphs one has to appreciate that cardiac arrest is a disease with an extremely rapid course, measured in minutes. From the moment of collapse, the clock of resuscitation starts to tick. By 8 minutes if there is no therapy the potential for resuscitation falls to zero. See Figure 5.7. As noted above the maximum potential for prehospital resuscitation is set at 50%. This is somewhat arbitrary and the exact ceiling may be higher. But for illustration purposes this ceiling is less important than the influence of various therapies.
Rapid provision of CPR alters the potential for survival by slowing the dying process. If CPR begins at 4 minutes the process is slowed but survival will still fall to zero since CPR by itself will not achieve a life sustaining cardiac rhythm. Letís assume defibrillation is delivered at 6 minutes. Since defibrillation is definitive therapy for VF the maximum survival is defined by when this therapy is delivered. In the theoretical illustration of Figure 5.7 survival of 20% can be attained if CPR begins in 4 minutes and defibrillation is provided at 6 minutes. This rate can be boosted even higher with good interaction of CPR and defibrillation, with timely arrival of paramedic care. (What do I mean by timely? I think paramedics should arrive within 5 minutes of EMTs at least 50% of the time. This 5 minute target assumes that the EMTs are providing quality CPR and one or more shocks to the patient.). Yet another way to improve the overall survival is with early institution of hypothermia. Each of these additional factors (good interaction of CPR and defibrillation, rapid arrival of paramedics, institution of hypothermia) may increase survival another 5%.
The cardiac arrest survival formula is particularly useful in identifying areas needing improvement. How to improve these areas is another matter and discussed in Chapter 10. To address this challenge it should be apparent that many of the system and therapy factors are contributory and directly influence the determinant factors. It is common sense that to solve a big problem you have to break it down into its component (or contributory) parts. Improve the parts and the big problem will take care of itself. Viewed this way the task becomes more manageable. If a fire chief were given a mandate from the mayor to shave 2 minutes off the time from collapse to defibrillation and 1 minute off the time to CPR, such a task on first blush would appear overwhelming but if 4 or 5 contributing factors could be identified the task changes from impossible to difficult. In order to meet the mayorís order, the fire chief might consider any of the following: A rapid dispatch program to insure quick response of the first-in unit and thereby a quick time to CPR; digital voice recordings at resuscitations to reconstruct the sequence of events and identify possible correctable delays in therapy; an aggressive telephone CPR program to increase the rate of bystander CPR and therefore a shorter average time to CPR; strong medical leadership to supervise proper protocol adherence; and establishment of a 60 second standard for time from arrival at patient side to first shock. Thus the secret to success lies in improving the contributory factors which in turn will improve the determinant factors. (Figure below)
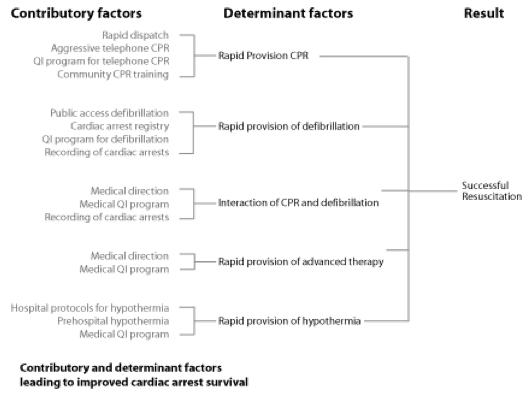
Quality improvement is a common denominator among the contributory factors. All the determinant factors are influenced by and nurtured by QI. At its essence QI is simply the tool to measure if performance is meeting expectations and if intended improvements are working Ė are things getting better, worse, or staying the same? An EMS system without an active and vigorous QI program is like a mountaineer without a compass.