System Factors
System factors refer to the organization, practices, and delivery of EMS care in that community. These include: time from collapse to CPR, quality of CPR, time from collapse to defibrillation, quality of defibrillation, interaction of CPR and defibrillation, type of EMS system, system size, number of responders, ratio of paramedics to population, use of dispatcher-assisted telephone CPR, quality of EMS care, quality of medical direction, on-going medical QI program, organizational structure and culture, administrative support, quality of training, community programs to teach citizens CPR, and community programs to encourage public access defibrillation.
| System Factors | Strength of Association with Outcome |
| Time to CPR | ++++ |
| Quality of CPR | ++ |
| Time to defibrillation | ++++ |
| Quality of defibrillation | Unknown |
| Interaction of CPR and defibrillation | +++ |
| Type of EMS system | ++ |
| System size | Unknown |
| Number of responders | Unknown |
| Ratio of paramedics to population | Unknown |
| Dispatcher-assisted telephone CPR | +++ |
| Quality of EMS care | Unknown |
| Quality of medical direction | Unknown |
| On-going medical QI program | Unknown |
| Organizational structure and culture | Unknown |
| Administrative support | Unknown |
| Quality of training | Unknown |
| Community CPR training | ++ |
| Community public access defibrillation | ++ |
Time to CPR (strong association with survival):
Time from the moment of collapse to the provision of CPR is one of the strongest predictors of survival. Note however that the survival is relatively constant for the first 4 minutes. This flat part of the curve in the early minutes of the cardiac arrest probably reflects the fact that the body still has oxygenated blood. Once this oxygen is used up – probably by 4 minutes – the fall in survival relentlessly begins at the rate of approximately 5% per minute. This differential survival (high for the first four minutes then a rapid fall) is explained in a three phase model of cardiac arrest proposed by Myron Weisfeldt and Lance Becker. The first phase is called the electrical phase and it lasts approximately 4 minutes. Defibrillatory shocks are all that is needed during this phase and CPR is of lesser importance. The second phase is the circulatory phase. CPR is very important during this phase as it restores oxygenated blood to the brain and other organs. The circulatory phase probably lasts from the fourth minutes until minute 10 or 12. The last phase is the metabolic phase. Therapy during this phase is not effective (at least with our current science) because cellular damage has occurred beyond the point of modern science. Perhaps hypothermia may be of benefit during the metabolic phase. Support for the three-phase model came from Christie Gilmore who demonstrated no benefit from early CPR for VF cardiac arrest but a considerable benefit from 4 to approximately 12 minutes.
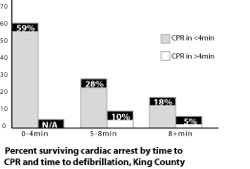
The figures demonstrating the importance of time to CPR and time to defibrillation are additive. Clearly the best scenario is one in which both times are short. Conversely the worst scenario is one in which both times are long. The relationship of the two times is shown in the table below. (Figure 5.6)
Quality of CPR (moderate association with survival):
One naturally assumes that the quality of CPR is important and several studies from the mid 1990s seemed to confirm this. In fact, however, this is a very difficult factor to study. For one thing, there are few cameras at the scene. For another it may be that minimal quality of CPR may be as good or almost as good as letter-perfect CPR. Despite these challenges, Tom Aufderheide in Milwaukee indirectly demonstrated the negative relationship of outcome and quality of resuscitation. In his study he had an observer monitor the number of ventilations provided by EMTs. The key finding was that EMTs compressed the chest too fast and gave too many ventilations. There were no survivors among the 13 cardiac arrests observed. Aufderheide and colleagues then went on to study the effect of too much ventilation in a pig cardiac arrest model. They demonstrated that over ventilation lead to a fall in blood pressure due to too much air in the chest preventing an adequate return of blood to the heart. Thus poor quality of CPR (in this case too much ventilation) can decrease the likelihood of successful resuscitation.
Another report from the 2007 Resuscitation Science Symposium of the American Heart Association demonstrated that incomplete chest recoil during CPR worsens hemodynamics. The study was performed in piglets but the findings were pretty convincing that leaning on the chest during CPR and not allowing the chest to fully expand on the upstroke led to worse systolic blood pressure, worse coronary perfusion pressure, and substantially reduced myocardial blood flow. The quality of CPR, probably because it was difficult to measure in clinical situations, has been an underappreciated factor and is only now beginning to emerge as an important aspect of successful resuscitation.
Technology may come to the rescue on the matter of CPR quality. Current defibrillators offer the ability to assess the quality of CPR during an actual resuscitation and verbally coach the rescuer to slow down or speed up compressions, compress deeper or not so deep, and give fewer or more ventilations. Future defibrillators may even be able to determine the volume of ventilations. This newer generation of defibrillators provides immediate feedback as well as records the quality of the CPR so it may be reviewed by the medical director.
Other devices, some currently available only in hospital settings, may one day play a role in assessing the quality of prehospital CPR. For example, echocardiography may be able to determine the quantity of forward blood flow associated with CPR and even determine if there is a mechanical impediment to adequate blood flow.
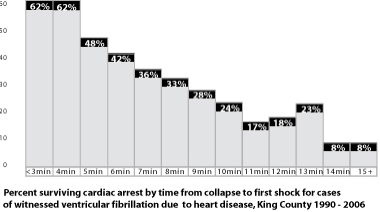
Time to defibrillation (strong association with survival):
Time from collapse to defibrillation is arguably the single most important predictor of survival. As seen in Figure 5.5 this relationship is striking. With each minute of delay in defibrillation the likelihood of survival falls by 5%. Note that survival does not fall for the first 4 minutes. This probably reflects the same phenomenon as was seen with time to CPR. The body is well oxygenated for the first four minutes following cardiac arrest and defibrillation is equally effective in the early minutes of cardiac arrest. The benefit of defibrillation can be modified by other factors. The most important is CPR. The early onset of CPR appears to extend the time in which defibrillation is effective. In this regard CPR slows the dying process. However, defibrillation when given very early after collapse may be all the therapy that is required. As the time to defibrillation increases more therapy is likely to be required. This therapy may be additional shocks, intravenous medications such as epinephrine and lidocaine or other rhythm stabilizers such as amiodorone or beta-blockers.
The figures demonstrating the importance of time to CPR and time to defibrillation are additive. Clearly the best scenario is one in which both times are short. Conversely the worst scenario is one in which both times are long. The relationship of the two times is shown in the table below. (Figure 5.6)
Quality of defibrillation (unknown association with survival):
Much like the quality of CPR is being appreciated as an important factor there is some evidence to suggest that the quality of defibrillation is also important. Quality here refers to the actual mechanics of operating and attaching the defibrillation. An abstract from the 2007 Resuscitation Science Symposium looked at where the electrode pads were placed on the chest and found that the placement location affected the measurement of VF amplitude. In other words pads that were not in the correct location could falsely conclude that VF is not present when in fact it is. This study was performed in humans who were undergoing implantable defibrillator procedures. As part of the procedure VF is induced in the patient as a means to test the implantable defibrillator. This provocative study suggests that proper training leading to proper placement of the pads may be an important factor.
Interaction of CPR and defibrillation (moderate association with survival):
Data from animal studies suggest that there is an important interaction between CPR and defibrillation. In other words, the sequence and timing of the two are emerging as important factors in resuscitation. It used to be taught in cardiac arrest protocols that the most important part of defibrillation was to deliver the shock quickly and often. The mantra was “shock fast and shock often”. But this old mantra has been replaced with “shock wisely”. Animal studies have revealed that the left ventricle quickly drains of blood when CPR is delayed or stopped. If a shock is given to a heart drained of blood there is no pressure to fill the coronary artery (called the coronary artery perfusion pressure). And if the coronary artery is empty of blood a shock will not be successful. The lack of blood deprives the heart of oxygen and the blood that is present may be very acidotic. The shock may work for a second or two but the heart will not stay defibrillated because there is no oxygenated blood in the heart muscle (because the coronary artery is empty because the left ventricle is empty because CPR is delayed or stopped). Rea and colleagues in King County observed that the old protocols resulted in long periods without CPR and as a result changed the cardiac arrest protocol for VF to minimize the no-CPR time. Delivering multiple shocks of up to three in a row (called stacked shocks) was eliminated and stopping for pulse checks after a shock was eliminated. A new protocol required one shock followed immediately by two minutes of CPR and then a reassessment of the rhythm. The goal was to provide CPR as much as possible between single shocks. The results were dramatic. Survival from witnessed VF went from 33% using the old protocol to 46% (p <.05) with the new protocol. This new protocol is in fact the one adopted by the American Heart Association at its 2005 international guidelines conference. Thus the entire nation is now using this new protocol and one hopes that survival is improving nationally.
Still to be settled is whether CPR should always precede the first defibrillatory shock. For example, if there is no bystander CPR and the fire department is first on the scene should they start CPR first of defibrillate immediately? Back in the early 70s it was dogma that CPR should precede defibrillation to “prime the pump” and rid the heart of lactic acid. By the 80s there was a growing body of information to suggest that time to shock was the best predictor of outcome and so a defibrillatory shock became the priority and was to be given as rapidly as possible. But recent studies from Seattle and Oslo(46, 47) questioned whether CPR should be given for several minutes prior to defibrillation. Both studies concluded that CPR provided by EMS personnel (for 90 seconds in Seattle and 3 minutes in Oslo) prior to defibrillation improved survival compared to patients who received a shock as quickly as possible. However, the scientific methodologies for both studies do not provide definitive proof -- the Seattle study was a before and after design and the Oslo study demonstrated a benefit only in a small subset of patients. To add further weight to the camp arguing for quick defibrillation a third study from Perth, Australia randomized immediate defibrillation or defibrillation after 90 seconds of CPR to 256 patients. The investigators found no difference in survival between the two groups. Thus, the best approach is unclear. There is a large North American on-going randomized clinical trail that is studying this very issue as part of the Resuscitation Outcomes Consortium.
It may well sort out that both approaches are correct -- immediate shock for witnessed VF or VF of short duration and CPR prior to shock for VF of longer duration. But while this debate rages the defibrillators are advancing to where the debate may become irrelevant. A new generation of defibrillators that guide therapy is beginning to emerge. Such a defibrillator will interpret information within the VF signal and advise immediate shock or a period of CPR and/or medications prior to the shock. Despite the appeal of such devices they have yet to be proven effective in human prehospital use.
Type of EMS system (moderate association with survival):
EMS systems can be characterized in many ways: private, public, fire department based, health department based, police based, single tier, or tiered response. There are no studies that compare the administrative structures to outcomes from cardiac arrest. There is only one study that indirectly compares single tiered systems to tiered response systems. In 1990 my colleagues and I compared 29 EMS systems that reported cardiac arrest survival and noted a strong relationship with type of system to survival. Systems that utilized paramedics as a single tier reported an average survival of 17% for ventricular fibrillation. This compared to an average of 29% for the systems utilized a tiered response of EMTs capable of defibrillation and paramedics. Presumably the difference in survival was due to the ability to deliver certain therapies (such as defibrillation) in a timely fashion. One must take such a study with a giant grain of salt. Since there were likely many differing factors and variables among the communities (such as rural versus urban, varied response times, age and co-morbidity differences) a direct comparison must be very qualified. The only definitive way to compare systems would be to have identical communities and randomly assign the type of system. But such a study would be impossible.
Tiered-response systems vary in terms of number of responders. A common approach utilizes an aid-unit as the first-in vehicle staffed with two (sometimes three) EMTs. The second-in unit is a paramedic-unit staffed with two paramedics (or one EMT and a paramedic). In this system both vehicles are capable of transporting the patient to the hospital. But there are many variations on this theme. Some communities may send a fire engine as the first-in vehicle (not capable of transporting the patient) and the second unit being a paramedic unit. Other communities may send three vehicles to a cardiac arrest: an engine company, an EMT unit, and a paramedic unit.
The Ontario Prehospital Advanced Life Support (OPALS) study measured the benefit of adding a paramedic program to an existing program of EMT defibrillation. This study did not demonstrate a benefit of paramedic services. Experience of the paramedics (or relative lack of it) and specific protocols may explain this negative finding. Contrary to the OPALS findings adding paramedic to existing EMT services in King County dramatically improved cardiac arrest survival. Paramedic services led to a survival of 28% for VF cardiac arrest compared to 15% when basic EMTs provided care. When this study began in 1976 basic EMTs were not authorized to defibrillate. It was clear that basic EMT services (without the authorization to defibrillate) alone saved considerably fewer lives in VF arrest compared to paramedic services (fortunately EMT services without defibrillation capability no longer exist). Over a 30-year period it is clear that in King County progressive levels of skills and services added to the EMS system have increased survival rates for VF. Basic EMT (without the authorization to defibrillate) services achieved the lowest survival rates. EMTs trained to defibrillate (the current training for EMTs) without paramedics achieved intermediate survival rates for VF cardiac arrest. And the tiered response system with EMTs (able to defibrillate) providing the first-in care and paramedics providing the second-in care achieve the highest survival rates.
Size of System (unknown association with survival):
Is there an optimal size for EMS programs? There is indirect evidence that small and rural communities and mega urban communities have lower survival rates than mid-size communities. This may reflect the logistics of getting EMTs and paramedics to the scene quickly. Factors such as housing density, high rise versus single family dwellings, and traffic congestion are all related to urban density. There may also be an optimal size when it comes to sphere of authority, a managerial term used to describe the ratio of supervisors to field personnel. Fire departments, based as they are on a military model, are generally able to create adequate supervisory staffing. The situation with medical direction is more problematic in large communities. Can one medical director know and supervise hundreds of personnel? In King County there is one county medical director, 6 paramedic program medical directors (serving a combined population of almost 2 million), and each base-station hospital has the emergency department physician on duty providing line control to the paramedics. None of the 7 directors works full-time as medical director and all have other responsibilities. Not counting the on-line emergency department physicians there are a total of 2 FTE physician directors (adding up the part time portions of the 7 physicians) supervising 250 paramedics in a community of less than 2 million people. For us this works well: one FTE medical director per 125 paramedics and approximately one million people. However, there are no data to suggest what an optimal sized system should be.
Number of responders (unknown association with survival):
Some researchers speculate that a critical mass of EMS providers leads to better cardiac arrest outcomes. A cardiac resuscitation should unfold like a choreographed dance with each individual performing assigned tasks. The concept of a critical mass means that each skill can be accomplished by a preassigned individual without the chaos of multitasking. For example, in tiered response systems the first arriving EMTs perform CPR and provide an initial defibrillatory shock(s) (a third EMT if present will take charge of the AED) When the paramedics arrive the lead (generally the paramedic not driving the vehicle) immediately takes charge. He or she starts the peripheral or central line in the patient and orders the medications. Meanwhile the other paramedic on arrival places the endotracheal tube and draws up the medications. It seems logical that sufficient personnel will achieve better outcomes compared to understaffed situations but there are no data to shed light on this matter.
In Seattle and King County there are usually three vehicles sent to the scene if the dispatcher thinks a cardiac arrest has occurred. The first-in unit may be a fire engine (staffed usually with three EMT fire fighters and dispatched because it is the closest vehicle) and the second vehicle is an EMT unit. This allows CPR (and defibrillation) to begin as quickly as possible, while the third vehicle, the paramedic unit, is enroute. Such a luxury of personnel offers allows for an efficient division of labor.
Ratio of paramedics to population (unknown association with survival):
The number of paramedics is related to the type of EMS system. Some communities utilize a fire fighter-paramedic system whereby paramedics respond to every 911 call. There are variations on this approach with private paramedics or a combined team of EMT and paramedics responding instead of fire fighters to every EMS call. In these systems there are many paramedics resulting in a high ratio of paramedic to population. Other programs utilize a tiered-response system (described above) whereby fire fighter-EMTs respond to all calls and paramedics only respond to calls where advanced skills are needed. These systems have fewer paramedics and a low ratio of paramedics to population. Bob Davis a reporter at USA Today conducted a survey or 50 American cities and concluded that too many paramedics in a community dilutes the opportunity to perform critical skills and ultimately leads to degradation of performance. This is an attractive concept but there are no studies of this relationship.
Dispatcher-assisted telephone CPR (moderate association with survival):
Dispatcher assisted telephone CPR has the opportunity to instantly instruct someone who has never had a CPR class as well as someone who needs a refresher on what to do. I am a strong believer in the benefit of telephone CPR. In King County this program led to a 50% increase in bystander CPR. Bystander CPR occurs in over half of all cardiac arrests and probably one-third of bystander events are solely due to the telephone CPR program. Though theoretically 100% of cardiac arrests could have telephone CPR delivered this in reality is impossible. Many calls occur as third-party relays. For example, the caller is a security guard in the lobby of the building and the event is on the 8th floor. Or the collapse may happen too far from a phone to offer instructions. Plus sometimes the caller is too frail or the victim cannot be moved flat on the floor. It is not possible to prove that telephone CPR saves lives since a resuscitation event has many interventions and it is often impossible to tease out the influence of each separate factor. Nevertheless in a large community study Rea demonstrated the strong association of telephone CPR with increased survival. Clearly time from collapse to CPR is a determinant of survival and it logically follows that telephone CPR is a means to insure increased bystander CPR. The only valid question is whether the quality of bystander CPR is as good as CPR taught in the traditional classroom setting. From simulations using manikins it appears that the quality is comparable.
Quality of EMS care (unknown association with survival):
There have been almost no studies on the quality of EMS care. (EMS care as used here comprises all the prehospital components of an EMS system including dispatching, EMT, and paramedic services.) This is not for lack of wanting. But in practice it is nearly impossible to agree on how to measure quality. One surrogate for quality is experience and here too there are almost no data. One study from England showed that the chances of cardiac arrests survival increased among EMTs with 4 years of experience and among paramedics with one year of experience compared to those with less experience. It seems intuitively correct that experience matters, especially on such skill-based activities as defibrillation, intubation and administration of intravenous medications. Though the data showing this relationship are slim, agencies could pair newly minted EMTs and paramedics with experienced partners for some period of time.
Another possible surrogate for quality is the degree of attrition within an EMS agency since low attrition is directly related to experience. A survey in JEMS of EMS salary and workplace factors found that fire departments had a low annual attrition of 6% compared to 17% in private ambulance agencies. Still another factor that may be related to quality is the salary paid EMS personnel. The same JEMS survey found the average salary of fire department based EMS to be $37,500 compared to $23,000 for private ambulance EMTs. Fire department paramedics received $42,000 compared to $32,000 for private ambulance paramedics. I do not know whether fire department EMTs and paramedics deliver higher quality care than private ambulance personnel since such data do not exist. Instead I am only pointing out the large salary differences and wondering whether salary in turn is related to quality of care.
Quality of medical direction (unknown association with survival):
There are no studies measuring quality of medical direction and outcomes from cardiac arrest. The main challenge is how to define quality of medical direction. Without this definition it is impossible to discriminate quality medical direction from mediocre or even poor direction? Is it full-time involvement? Is it personal review of critical EMS calls? Is it supervision of the cardiac arrest registry? Is it frequent visits to the paramedic stations and riding on calls? The matter of defining quality medical supervision is not unlike the challenge of defining quality performance in any service profession whether it be police, fire or utility services. I personally believe the amount and quality of medical supervision is directly related to the overall quality of an EMS system. But I cannot prove this.
On-going medical QI program (unknown association with survival):
Like many other factors in this list there are no studies directly liking an ongoing medical QI program to increased survival from community cardiac arrest. Nevertheless, on-going medical QI is part and parcel of a quality program. The medical director uses medical QI to measure skill performance and identify educational needs. An ongoing cardiac arrest surveillance program and an ongoing telephone CPR monitoring program are in essence medical QI. Most of the communities cited in the first chapter with the highest survival rates from VF cardiac arrest have active cardiac arrest surveillance and QI programs. Ongoing medical QI is a concrete recognition by the medical director and administrative director that a system has to continuously monitor itself and strive to do better.
Organizational structure and culture (unknown association with survival):
There is a large literature on management, organizations, and culture. There is, however, nothing that I am aware of that relates EMS organization and culture to cardiac arrest survival rates. One assumes that a well run organization and one with high expectations of excellence would perform better than organizations lacking these qualities. Most EMS agencies are based in fire department. By their very nature, fire departments are quasi-military organization; even the ranks are based on military ranks – chief, battalion chief, captain, and lieutenant. But quasi-military does not mean autocratic or dictatorial. A good organization, whether it be a fire department or a Fortune 500 company, encourages internal communications, values the experience of workers, and instills a sense of mission in the group.
Just like character helps describes an individual, culture can describe an organization. The perfect EMS culture should have the facets of professionalism, uncompromising standards, high expectations, and relentless drive to improve. The term culture of excellence summarizes these facets. Culture is different than pride. Many medical directors, dispatchers, EMTs, and paramedics are proud of their system and the hard work they do. Culture defines a quality that permeates and percolates throughout an organization. It begins at the top with medical direction and the administrative director and is instilled in every member of the agency. Members who don’t buy into the culture may be ostracized in subtle or not so subtle ways and often leave. Thus a culture has a tendency to perpetuate itself – this is good when the culture is one of excellence but not so good when a negative culture exists.
Administrative support (unknown association with survival):
Administrative support refers to the staffing and budget devoted to such matters as cardiac arrest registry, medical QI program, and data infrastructure. As with quality of medical care there are no data relating administrative support to cardiac arrest outcomes. Clearly if a community is to measure its performance it will require resources to do so. I cannot define what this level should be. In King County there are several employees dedicated to maintaining the registry and QI program. And at least 3 full time staff members are assigned to the overall data base of EMS incidents. But even more important is the full support from the top administrator whether he or she is the fire chief or the EMS director. Without this support no amount of staff will succeed in this task.
Quality of training (unknown association with survival):
Few would argue that quality of dispatcher, EMT, and paramedic training is a crucial ingredient in a successful EMS program. The challenge is how to define quality training. There are no studies measuring the relationship between the quality of training and outcomes from cardiac arrest. One can certainly measure the number of hours required for certification and recertification and the types of training – didactic versus practical skills, online versus face to face. In Seattle and King County dispatchers, EMTs and paramedics have extremely high training and continuing education requirements compared to national standards. Washington State, and Seattle and King County in particular, have the highest number of hours of required paramedic education in the nation. I suppose one could rank order or score systems based on the training hours or other performance measures. But the challenge is to isolate training as a factor and associating this with survival. Because quality of training is associated with other factors (such as culture, quality of medical direction, administrative support) it is difficult to tease out the independent contribution of training.
Community CPR training (moderate association with survival):
The Seattle Medic One program pioneered the concept of training citizens in CPR. It was recognized early on that the sooner CPR began the better the outcome. The concept was a simple one – if you train enough citizens then the odds of a trained person at the scene will increase. The program to train citizens in CPR began in 1971 and set a target of 100,000 trained individuals. This goal was attained long ago and it is estimated that almost 800,000 people in Seattle and King County have received CPR training. (Never trip and fall on the street in Seattle or someone will pounce on you and begin CPR. Or so the urban legend goes.) This large number of citizens accounts for the consistently high rate of bystander CPR in Seattle. Before the dispatcher assisted telephone CPR program began in 1988 the rates of bystander CPR averaged 30-40% per year. With the telephone CPR program this rate is over 50%.
The American Heart Association endorses dispatcher assisted telephone CPR and many dispatch centers, if not most, offer this assistance. But as the expression goes, there are dispatcher CPR programs and there are dispatcher CPR programs. Without dedicated staff to monitor and review the calls and provide constructive feedback to the dispatchers, the program can easily become one of unmet expectations. Several proprietary telephone CPR programs exist as part of a comprehensive computer aided dispatch program. These proprietary programs have neither been evaluated nor validated. My concern is whether they deliver the key steps of CPR quickly enough and whether the exact wording of the instructions leads to the expected performance. Each proprietary program should publish its performance for several key indicators. For example, how quickly does the dispatcher recognize the presence of cardiac arrest? What is the average time from call pick up to first ventilations and to first compressions? What percentage of cardiac arrests calls have instructions offered by the dispatcher? What is the false positive rate for delivering telephone instructions? When every second counts it is important that the telephone instructions be as effective and efficient as possible.
Community public access defibrillation (moderate association with survival):
The public access defibrillation trial demonstrated that automated external defibrillators in public locations can improve cardiac arrest survival. This large randomized trial proved the concept that an AED at the scene can save valuable time to defibrillation.(26) This time saving directly translates in higher survival rates. In Seattle and King County there is an active program to encourage and register AEDs in the community. Each AED is listed with the local dispatch center so callers can be reminded of the presence of an AED. Linda Culley and colleagues at King County studied the initial community experience with these AEDs. There were 50 episodes when an AED was used before the fire department arrived. Survival in this cohort was 50%. While public AEDs offer the opportunity to shave time from collapse to defibrillation one has to put the potential benefit in perspective. Only 15% of all cardiac arrests occur in public locations. Furthermore some public locations are more likely to have a cardiac arrest happen. Airports, jails, health clubs and shopping malls have the highest incidence of arrest and are logical places to place AEDs and train staff to use them. Despite the relative low number of public cardiac arrests compared to arrests in homes the public events are far more likely to be witnessed and to be in ventricular fibrillation. Thus the relative impact of community defibrillation is far greater than the numerical proportion of public cardiac arrests. An active community defibrillation program can make a significant contribution to a community’s VF survival rate.