Measuring time intervals
Accurate measurement of time intervals involved in cardiac arrests is very challenging. Although some of the intervals can be precisely measured others are more problematic. Ideally one would like to know the time of collapse and the time of key interventions such as CPR and defibrillation. The collapse of the patient in cardiac arrest is the anchor time that starts the therapeutic clock. (Of course, when the collapse is unwitnessed it is impossible to determine key time intervals and for this reason most communities do not attempt to measure time intervals for unwitnessed cardiac arrest.) Even in a witnessed collapse it is not possible to know the exact moment of collapse. In King County we arbitrarily assign one minute to this down time (time from collapse to calling 911) unless the caller gives a concrete reason for delay. Some examples are "running next door to get my neighbor", "calling my doctor", "couldn't find the cordless phone".
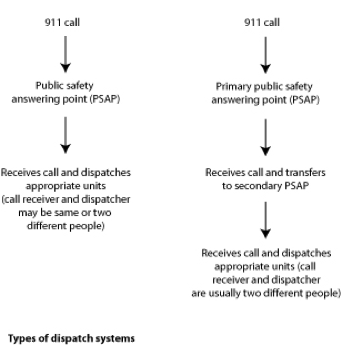
Most EMS systems document the time of the 911 call. This may not appear as straightforward as it seems. For one thing if the call rings for a long time the dispatch center only registers the pick-up time. A second problem is that many communities route the 911 call to a PSAP - public safety answering point - which then routes the call to the secondary PSAP, the fire department or EMS dispatch center. It is near impossible to link the call time at both centers and thus the routing time from the primary PSAP to the secondary PSAP is usually lost in any analysis of time. But let's assume this routing time is 30 seconds or so.
Next is the response time. Again what should be straightforward is filled with complexity. This time ideally should be the interval from the dispatch center alerting the EMTs and paramedics to the arrival at the patient's side. But most communities report this as the interval from the personnel responding to arrival at or near the address. This doesn't take into account the time to gather the team on the front end or the time from arrival at the address to carry equipment and reach the patient's side at the back end.
Next we have the problem of determining when CPR begins. When a bystander starts CPR it is impossible to anchor this time. Sometimes dispatcher-assisted telephone CPR can define a start time but few if any centers routinely record this time. Even when EMTs are the ones to start CPR this time is not recorded.
Last there is the exact moment of defibrillation. All current defibrillators and AEDs time stamp the moment of defibrillation. Thus, easy as pie to compare this time with the call to 911 and accurately calculate the time to defibrillation. Wrong. Few EMS programs synchronize their AEDs or defibrillators with the alarm center times. The Table lists the common times associated with cardiac arrests
| Times and Intervals Associated with Cardiac Arrest | |
| 1. Collapse time | Precise moment of collapse |
| 2. Down time (access time): | Time interval from collapse to call 911 |
| 3. Ring time | Time interval of 911 phone rings |
| 4. PSAP pick-up time | Precise time of 911 operator answering phone |
| 5. PSAP process time | Time interval to transfer call to secondary PSAP |
| 6. Secondary PSAP ring time | Time interval of secondary PSAP phone ring |
| 7. Secondary PSAP pick-up time | Precise time of secondary dispatcher picking up phone |
| 8. Secondary PSAP process time | Time interval for dispatcher to decide which personnel to send |
| 9. Dispatch time | Precise time of dispatch |
| 10. Muster time | Time interval to gather the team and respond |
| 11. Roll time | Precise time vehicle starts to move |
| 12. Response time | Interval from 3, 4, 7, 9, or 11 to arrival at address |
| 13. Arrival time | Precise time of arrival at address |
| 14. At-patient time (scene time) | Precise time of arrival next to patient |
| 15. Time to CPR | Ideally time interval from 1 or 3 to beginning of CPR |
| 16. Time to defibrillation | Ideally time interval from 1 or 3 to first shock |
PSAP stands for public safety answering point
Though I have tried to select commonly used terms, there are no agreed upon definitions for these time intervals; different terms may be used by various EMS agencies. The time intervals are shown in the Figure below. Time intervals are given only as examples.
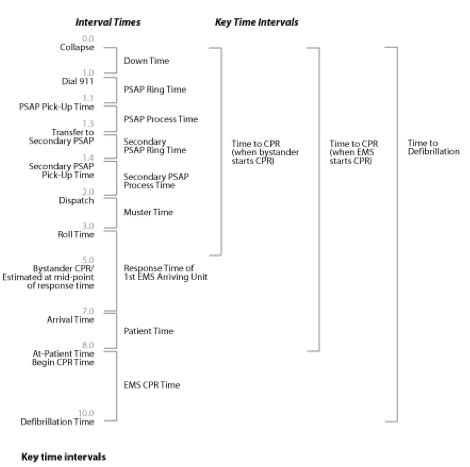
Many researchers in EMS make no attempt to determine the down time and instead start the clock at the dispatch time. There are valid reasons for this not the least of which is the fact that the moment of collapse can only be estimated. Better to start with a concrete time than an estimated time. And the early portions of the 911 call cannot usually be linked or are difficult to obtain, especially if two PSAPs are involved. This is regrettable since exclusion of the down time gives an inaccurate portrayal of the event. Most systems with concerted effort can at least define the pick-up time (usually time stamped at the alarm center) of the primary PSAP and the secondary PSAP. This pick-up time at the primary PSAP defines the front end anchor of the objective times. For systems without resources to estimate down time, I think it is reasonable to "start the clock" at the PSAP pick-up time. One has to assume that down times on average are approximately one minute.
Defining the time of defibrillation requires daily synchronization between the defibrillator and the alarm center. This is not very high-tech but it solves the problem of being able to define this key interval. When EMTs start CPR the time to CPR is usually the at-patient time plus a fixed interval of 60 seconds (it takes about one minute to set up equipment and position the patient). When bystanders start CPR estimating the time is more problematic. Since one cannot precisely know when bystander CPR begins an estimate is to use half of the interval from call pick-up time to the at-patient time. Estimates are of course compromises but the alternative would be to throw out the data entirely. My biostatistician colleagues tell me that new techniques (termed imputation of data) can account for using a combination of accurate and estimated intervals when relating times to survival. Regrettably most programs continue to report their systems performance based on simple response times. In many programs response time is the time from wheels rolling until arrival at the address of the alarm. Such a policy completely underestimates the true time intervals from collapse (or PSAP pick-up time) to key interventions. The systematic inability to precisely measure critical time intervals would be comparable to building a 747 aircraft and measuring the parts with a ruler accurate to the inch instead of the micron. The plane would fall apart as it taxied down the runway. Stated quite simply, one cannot begin to assess the quality of an EMS system without detailed and accurate knowledge of critical time intervals.
There are promising developments in the dispatching world. A national effort championed by the Department of Transportation, termed NG911 (NG stands for next generation), will bring dispatching into the 21st century and solve many of the problems inherent in tracking calls between primary PSAPs and secondary PSAPs. The 911 system of the 1970s, created for voice media only, cannot easily accommodate new wireless and multimedia technologies. NG911 network is designed to identify and locate voice, text, pictures, and video emergency calls from any communications device via internet-like networks. The enhanced capacity of NG911 has the potential to accommodate run reports (including ECG, physiologic, and therapeutic information) and hospital clinical information for a particular resuscitation and integrate it into the dispatch data base thus creating a unified and detailed resuscitation report. There is as yet no timetable or funding for this promising technology.